What is “Ethnic” Skin?
While the term ethnic is something that has been widely used to describe individuals with darker skin, this is not always correct, as there are likely many more Americans who have a mixed hereditary background than those that are truly one ethnicity. The Fitzpatrick Scale, which was developed in 1975 by Harvard Medical School dermatologist Dr. Thomas Fitzpatrick, is a classification scale for identifying the color of a client’s skin. (See Figure 1.)
 Although the most apparent difference between the skin of those of differing ethnicities is, of course, its color, there are also variances in skin thickness, vascularity, and predispositions to certain conditions and diseases. Darker skin has a tendency to be more sensitive to irritation and heat, so it is wise to use this scale with each of your clients at the initial consultation. Although this scale is useful, it does not always alert the clinician to the potential for complications or common predispositions. One client can have skin that is a Fitzpatrick II or III and have a parent who is of an ethnicity that is more prone to hyperpigmentation, such as Indian or Asian. In addition to the Fitzpatrick Scale, always ask clients about their hereditary background so you are aware of any potential for unwanted pigmentation due to treatment – or to help you identify the reasons behind a particular skin condition.
Although the most apparent difference between the skin of those of differing ethnicities is, of course, its color, there are also variances in skin thickness, vascularity, and predispositions to certain conditions and diseases. Darker skin has a tendency to be more sensitive to irritation and heat, so it is wise to use this scale with each of your clients at the initial consultation. Although this scale is useful, it does not always alert the clinician to the potential for complications or common predispositions. One client can have skin that is a Fitzpatrick II or III and have a parent who is of an ethnicity that is more prone to hyperpigmentation, such as Indian or Asian. In addition to the Fitzpatrick Scale, always ask clients about their hereditary background so you are aware of any potential for unwanted pigmentation due to treatment – or to help you identify the reasons behind a particular skin condition.
Hormones and Pigment
In all ethnicities, there are certain factors in the pigment production process that are intricately tied to hormone activity; other areas are either exacerbated or complicated by the release of hormones.
Hormonally Driven Hyperpigmentation: Melasma
The primary type of hyperpigmentation that is inextricably connected with hormone function is melasma. The term “melasma” comes from the Greek word “melas,” which means black. It appears as large symmetrical bilateral patches with jagged and distinct borders, typically around the jawline, upper lip, cheeks, and forehead. Melasma is unlike sun-induced hyperpigmentation that is more dispersed and freckled in appearance.
Melasma is associated with a fluctuation of hormones and can affect patients of all ethnicities, although ethnic skin is more vulnerable. There are multiple times during a person’s life when hormone fluctuations may cause skin challenges, but pregnancy, oral contraception use, thyroid dysfunction, menopause or hormone replacement therapy (HRT) are the main culprits in the development of melasma. Although not instigated by ultraviolet (UV) exposure, it will worsen with sun exposure. The combination of UV radiation and hormone-related melanocyte stimulation will not only worsen the condition, but may allow the melasma lesions to remain visible for prolonged periods of time and potentially become persistent.
Higher Fitzpatrick skin types are typically more prone, and melasma is more prevalent in Fitzpatrick skin types IV and above. It has been demonstrated that there may be a hereditary link, making those with a family history more likely to develop this frustrating condition. Studies by dermatologist Susan Taylor in 2005 demonstrated that 86 percent of women of Latino and African descent are concerned about skin discolorations.
Potential Explanations
While the exact cause is unknown, melasma is thought to be a result of an increase in the formation and distribution of melanosomes (packets of melanin pigment) among the keratinocytes, along with increased branching of melanocytic dendrites. If there are more dendrites, there is an increased opportunity for melanin to be dispersed into the keratinocytes, exacerbating and intensifying the discoloration.
There are several additional considerations for this type of hormonally driven hyperpigmentation:
- Larger and intensely pigmented melanocytes
- An increased number of estrogen receptors within the affected melanocytes
- Increased amount of dermal and epidermal melanin
- Neurotrophin involvement in melanin synthesis
 Interestingly, it is not simply the surface of the skin where the melasma appears that is darker, but the melanocytes responsible for the melasma patch are themselves darker in color than normally functioning melanocytes. This is due to these estrogen-affected melanocytes hyperactively producing pigment. These melanocytes are also larger in size in areas affected by melasma than in those that are unaffected.
Interestingly, it is not simply the surface of the skin where the melasma appears that is darker, but the melanocytes responsible for the melasma patch are themselves darker in color than normally functioning melanocytes. This is due to these estrogen-affected melanocytes hyperactively producing pigment. These melanocytes are also larger in size in areas affected by melasma than in those that are unaffected.
Studies show there is typically a significant amount of redness involved with melasma, although it is difficult to see, in higher Fitzpatrick skin types. Anti-inflammatory products and treatments that reduce redness may be helpful and additionally reduce the risk of ethnic patients developing post-inflammatory hyperpigmentation (PIH) in addition to their melasma.
As mentioned, the causes of melasma are not yet fully elucidated, yet it is purported that the estrogen receptors play a role. Estrogen receptors are proteins that are activated by estrogen located in cells all over our bodies (kidney, brain, bone, heart, lungs, prostate, ovaries, endothelial cells, et cetera). When estrogen binds with these receptors, it causes the cell to grow. Some studies demonstrate that the melanocytes of melasma sufferers have an increased number of estrogen receptors than normally functioning melanocytes. With further study, if this proves to be true, it would certainly help to explain the link between hormonal fluctuations and melasma.
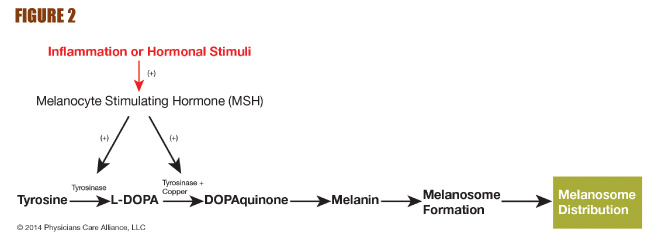
Neurotrophins are proteins that encourage the growth and function of neurons, or nerve cells; they are growth factors for nerve cells. Studies have found that neurotrophins not only encourage the growth of neurons, but that they also may play a role in the instigation of melanogenesis – the cascade of biochemical reactions that terminates in the deposit of pigment. (See Figure 2.)
Complicating Factor for Ethnic Skin
There are several mechanisms of melanosome transfer from the melanocytes to the surrounding keratinocytes, one such mechanism being phagocytosis. This is the process by which a cell engulfs and devours another particle. It can be a way in which cells acquire nutrients, but in the case of melanogenesis it involves the keratinocytes taking in or phagocytizing the melanosomes transferred from their adjacent melanocyte. The keratinocyte receptor protease-activated receptor-2 (PAR-2) controls melanosome phagocytosis by keratinocytes, playing a regulatory role in skin pigmentation. Protease-activated receptor-2 expression is increased in higher Fitzpatrick skin types, exacerbating their already increased predisposition for developing unwanted pigment. Protease-activated receptor-2 expression is also accelerated by UV exposure, making daily, year-round sun protection critical.
 Treating the Ethnic Melasma Patient
Treating the Ethnic Melasma Patient
Due to the hyper-responsive nature of the melanocytes in ethnic skin, paired with the accelerated production and transfer of melanosomes present in melasma, a gentle approach to treatment is an integral part of achieving a positive treatment outcome with ethnic melasma patients. It is essential to choose effective, yet gentle, combinations of home use products containing efficacious, yet non-irritating, melanogenesis-inhibiting ingredients coupled with superficial blended chemical peels to avoid over-stimulating the skin and instigating the production of post-inflammatory hyperpigmentation (PIH). Clearing melasma, in all ethnicities, is a challenging task. It typically takes longer to respond to treatment and persistence and patience is key. Council and educate ethnic melasma patients about the need for the skin to be treated gently to avoid worsening rather than clearing their condition.
Time-Tested Ingredient Choices
Because melanogenesis is a process with many interconnected reactions, effective treatment is achieved by using topical products containing ingredients proven to interrupt melanin production at multiple points simultaneously. This approach is especially helpful when treating hormonally driven pigmentation in ethnic skin, because it can help to resolve the condition more rapidly without irritation. A variety of over-the-counter (OTC) and cosmeceutical ingredients have shown the ability to facilitate clearing.
Hydroquinone (HQ) is the most prescribed skin-lightening agent worldwide. Hydroquinone suppresses the binding of copper and tyrosinase, thereby inhibiting tyrosinase activity. Studies have also demonstrated that hydroquinone decreases the formation and promotes the degradation of melanosomes, inducing melanocyte-specific cytotoxicity. Cosmeceutical products can contain up to 2 percent hydroquinone. Using these lower concentrations as opposed to higher, prescription strengths is an especially important step when treating higher Fitzpatrick skin types to avoid potential post-inflammatory hyperpigmentation. Prescriptions as high as 10 percent hydroquinone are dispensed by physicians, but this is especially important to avoid in ethnic clients, as this ingredient can be a strong surface irritant, especially at higher percentages. Patch testing all clients with hydroquinone prior to use is highly recommended. Kojic acid disrupts melanogenesis by chelating the copper bound to the tyrosinase. Kojic acid also decreases the number of melanosomes and melanocytic dendrites. There is a potential for contact dermatitis following kojic acid application; therefore, ethnic patients should be patch tested to avoid unwanted inflammation from treatments or product use. Lactic acid is a gentle, water soluble alpha hydroxy acid that increases exfoliation. The melanin-filled keratinocytes are lifted and removed, ultimately fading dyschromias. Lactic acid also suppresses the formation of tyrosinase, without which melanogenesis cannot occur. L-ascorbic acid is able to convert Dopaquinone back to L-dopa during melanogenesis, preventing melanin formation. L-ascorbic acid’s antioxidant, anti-inflammatory and UV-protective capabilities are also important to the suppression of melanogenesis.Retinoids, such as retinoic acid, retinol and retinaldehyde, inhibit tyrosinase to suppress hyperpigmentation and enhance cell turnover. Research has also shown that retinoids inhibit the over-production of neurotrophins. Retinol is typically used in cosmeceutical preparations, as it is successfully converted to retinoic acid within the skin. This is especially important for ethnic patients with sensitive skin, as prescription retinoic acid can be highly surface stimulating, potentially leading to post inflammatory hyperpigmentation. Azelaic acid inhibits tyrosinase activity and suppresses the proliferation of melanocytes. Arbutin is a natural derivative of hydroquinone that allows controlled release of hydroquinone into the skin. Arbutin also suppresses the activity of tyrosinase, inhibits melanosome maturation and provides antioxidant protection. Resorcinol derivatives, such as phenylethyl resorcinol, inhibit the conversion of tyrosinase to L-dopa during melanogenesis. Resorcinol derivatives are also antioxidants. Undecylenoyl Phenylalanine can avert the synthesis of the melanocyte-stimulating hormone (MSH) and, as a result, prevents the formation of tyrosinase and melanin, suppressing melanosome transfer.

Superficial Chemical Peels for the Ethnic Melasma Patient
Although many have the misconception that all chemical peels are aggressive and uncomfortable, there are gentle blended superficial peels that are highly effective but cause little to no irritation or inflammation. The melanin deposited in the skin due to hyperpigmentation will appear darker to the naked eye as it rises toward the stratum corneum on its way to being shed. Part of a successful melasma treatment plan is to remove these darker impacted cells to keep the appearance of the pigmented area to a minimum – even as you are working to increase cell turnover and lift deeper pigment to the surface. To keep the unwanted pigment from re-depositing on the surface, it is wise to perform a superficial peel every three weeks. Although this is a normal part of lifting pigment, if the stratum corneum is gently removed before it has a chance to become visibly darker to the client, they will be happier and typically will remain more compliant with the predetermined plan. Because inflammation is the direct trigger of hyperpigmentation, gentle exfoliation is crucial. If aggressive methods are employed, the condition will worsen, not improve. It is important to avoid high-percentage, straight acid peels and any mechanical methods, such as harsh scrubs or loofahs, to avoid post-inflammatory hyperpigmentation.
Broad Spectrum Protection
Last, but most certainly not least, is the reminder that all patients should follow a strict regimen of daily year-round sun protection. This should come in the form of a broad spectrum product with a sun protector factor of at least 30 every morning. There are now formulations available that also contain antioxidants to further mitigate the oxidative damage that is instigated by UV exposure. Although this is critically important for all clients, it is truly non-negotiable for the ethnic patient fighting melasma. Although melasma is not initially instigated by UV exposure, it is clearly worsened by unprotected exposure. By understanding the complex nature of ethnicity in today’s global melting pot and employing targeted strategies for combating the frustrating, hormonally driven condition of melasma, any clinician can provide their ethnic client base with gentle, effective products and treatments that deliver dramatic,
visible results.
 Jennifer Linder, M.D. serves as the chief scientific officer for PCA SKIN®, guiding all product development and clinical trials for the company. A board-certified dermatologist and a fellowship-trained skin cancer surgeon using the Mohs micrographic technique, Linder is one of the foremost United States experts in the use of the cosmetic filler, Sculptra. She holds a clinical faculty position in the Department of Dermatology at the University of California, San Francisco.
Jennifer Linder, M.D. serves as the chief scientific officer for PCA SKIN®, guiding all product development and clinical trials for the company. A board-certified dermatologist and a fellowship-trained skin cancer surgeon using the Mohs micrographic technique, Linder is one of the foremost United States experts in the use of the cosmetic filler, Sculptra. She holds a clinical faculty position in the Department of Dermatology at the University of California, San Francisco.
Want to read more?
Subscribe to one of our monthly plans to continue reading this article.