We are bombarded regularly by commercials and advertisements extolling the virtues of exfoliation. Products contain "micro-scrubbers", apricot pit grounds, and other ingredients touted to scrub away the outer layers of dead skin cells while "making skin appear fresh and beautiful." About a decade ago microdermabrasion was introduced, while chemical peels have been used for decades. Yet as exfoliation use is burgeoning, the incidence of skin cancer has continued increasing faster despite the introduction of high potency sunscreens (>SPF 15). Understanding the science behind exfoliation is important for any skin care professional in order to provide the best service to your clients.
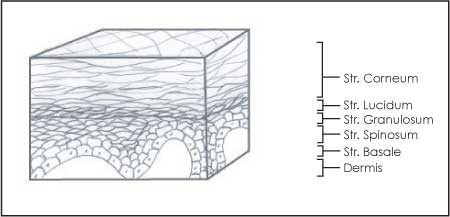
Let's begin with a brief lesson of skin physiology. The skin is comprised of three distinct layers: the subcutaneous layer (the deepest layer of fatty tissue), the dermis (the middle layer, where collagen and elastin and new skin cells are formed), and the epidermis (the outermost layers of the skin). The most superficial strata of the epidermis is the stratum corneum, which consists of several layers of dead skin cells (corneocytes) interspersed with multiple layers of three key lipids – cholesterol, ceramide, linoleic, and other free fatty acids. This skin barrier maintains the aqueous internal environment while keeping out harmful microbes, toxins, and allergens. New corneocytes are derived from maturation of dividing basal cells. Beyond age 65, the skin cell maturation process slows up to 50 to 60 days for newer cells to reach the surface rather than 28 to 32 days in young adults, which is why older skin can appear dull and waxy.
"Exfoliation" describes the process by which the top layers of stratum corneum cells are sloughed off. This process induces epidermal cell turnover via basal cell creation to maintain normal skin barrier function. A compromised skin barrier activates acute inflammation in the skin, which induces the synthesis of collagen, elastin, and ground substance for healing. As one ages, the repair process is disturbed leading to activation of chronic inflammation. This results in increased synthesis of the destructive enzymes – matrix metalloproteinases (MMPs) – that not only induce the dermal changes of visible fine lines and wrinkles but play a role in malignant transformation of skin cells. This process can happen either manually through scrubs or microdermabrasion, or chemically through chemical peels. The goal is to remove as much of the epidermis without inducing bleeding by staying above the dermal papillae. This depth also prevents scarring. Exfoliating the skin surface produces a visibly smoother and more vibrant appearance with resolution of the sallow, matte look. Texture is also improved and pigmentation irregularities tend to be blended and less distinct.
Manual exfoliation is the most common type of exfoliation. There are plenty of options available from drug stores around the world for use at home. These scrub products will include roughly-textured sponges or brushes, or grains and pit grounds to cause the exfoliation. However, these are often applied too aggressively and can be significantly more damaging to the skin than helpful by inducing superficial lacerations and abrasions that can activate destructive chronic inflammation. Within the skin care professional world, the use of more advanced manual exfoliators includes microdermabrasion (a surface "vacuuming" treatment that uses either blown crystals or a textured handpiece to resurface the skin), ultrasonic skin spatula (which uses a metal blade and ultrasonic vibrations to gently remove surface cells), and also dermaplaning (in which a #9 surgical blade is used to remove outer cells and vellous hair).
Chemical exfoliation comes in many different forms, beginning with certain protein-loving enzyme products that contain fruit-derived ingredients such as papain (papaya) or bromelain (pineapple) enzyme. Chemical peels utilize certain types of acids derived from fruit or other plants, such as 10 to 90 percent alpha-, beta-, or poly-hydroxy and trichloracetic (<25 percent) acids to disrupt the lipid layers and intercellular structures that hold the stratum corneum corneocytes and epidermal keratinocytes together. Tretinoin induces a form of chemical peeling. It is a vitamin A derivative which must be prescribed by a physician. Mid-depth peels with 35 to 40 percent performed under anesthesia by physicians include TCA (trichlorocetic acid) and deep phenol peels. Anesthesia or sedation may be required as is cardiac monitoring for phenol peels. These all have at least 10 days of staying indoors with weeping/crusting of skin. They also carry a risk of scarring and pigmentation abnormalities. Phenol peels may induce life threatening heart problems. These aggressive peels are being replaced by more intense resurfacing techniques performed under physician supervision encompassing the use of lasers, such as CO2 or fractional laser for better depth control to reduce side effects with improved results.
 Procedure Preparation
Procedure Preparation
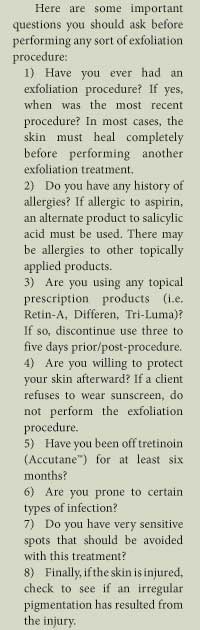
A pre-procedure program is equally as important as the exfoliating procedure itself. First, an analysis of skin type should be done. Understanding Fitzpatrick Skin Typing is imperative, and while it will not be covered in depth here, if you are not confident in your knowledge of this system, please take the time to do so. The Rubin classification of photodamage, which rates the level of sun damage in the skin (alterations in the epidermis and dermis) is equally important. Analysis of a client's skin using both of these systems will help you determine which type of exfoliating procedure will best suit the client's needs. Pre-treating the skin for two to four weeks with topical retinoids or a barrier repairing and inflammation prevention therapy are documented to improve healing and reduce side effects.
When using exfoliating procedures as adjunctive to medications, you must consider the disease severity and types of lesions. A client with acne grades 2+ (>10 lesions on each side of face) should consult with a dermatologist to consider oral prescription treatment options, and underlying hormonal disease. If a client has inflamed, pustular lesions, microdermabrasion should be avoided to prevent a flare response or spreading pathogenic microbes. A culture for bacteria and yeast should be performed. Rosacea must be treated very gently. Clients with a known or suspected history of oral herpes, fever blisters, or cold sores should be given a prescription such as Valtrex, acyclovir, or Famvir to prevent an outbreak after treatment.
It is also important to appropriately consult with the patient prior to the procedure taking place to determine realistic goals and expectations. Hereditary and current skin conditions as well as climate, season, and diet can all impact how well a client may react to the exfoliating procedure.
Appropriate procedure preparation will help improve the healing process for the skin during the healing phase of the exfoliation procedure, and will ensure that it is optimally beneficial to your client.
Procedure
The first step in an exfoliating procedure is to properly cleanse the skin. While this may seem to be a no-brainer, appropriate cleansing is critically important. The acid mantel within the stratum corneum protects the skin from infection. Acidic in nature, it has a low pH. This is important to keep in mind because it means that a cleanser must avoid disrupting this mantel by having a neutral pH. If you are unsure of a product's pH, contact the manufacturer prior to introducing it into your procedure protocol.
There are two reasons why exfoliation can do more harm than good long term. When the superficial strata are removed the more vulnerable newer cells are exposed to environmental insults such as UVA and UVB rays and pollution. When disturbed, the skin barrier takes up to 36 hours to return to its natural protective state. During this recovery time, the environmental insults are bombarding the newly exposed cells, continuing the chronic inflammatory process that can last for weeks beyond the actual procedure. The acute inflammation during the procedure itself is beneficial to encourage new cell rejuvenation and collagen, elastin formation, and matrix. The destructive chronic inflammation caused by environmental insults reduces the expected clinical benefit of the procedure.
Once the procedure is complete a skin care professional must apply a product that will rapidly repair and fortify the skin barrier in a timely fashion, i.e. before the client walks out the door and into the sun and pollution. Gentle cleansing and rinsing after the procedure is helpful. White petrolatum products or Aquaphor™ are commonly used products which produces 45 percent repair by 45 minutes after application.
The superficial procedure may be repeated every one to four weeks while the mid-depth peels may be used every two to four months.
Post-Procedure Treatment
In order to provide your client with the best service, a post-procedure program must be as important as the preparation and the procedure. Post-op care consists of applying a barrier repairing/inflammation prevention product for two to four days after the procedure. The client needs to be provided with the opportunity to purchase appropriate post-procedure products for at-home care. These products should include a pH neutral cleanser, a hydration and barrier-repair product, and sunscreen with a minimum of SPF 30. Depending on what type of exfoliating procedure is done will determine your recommendations to the client regarding the at-home regimen. Remind the client to not use at-home exfoliation products for at least 48 hours after the professional procedure, or until any residual irritation or peeling has stopped. Fabric hats should also be used for continued skin protection and healing. This is also an appropriate opportunity to encourage your client to make sunscreen use with broad spectrum protection and high SPF along with other lifestyle adaptations part of their daily routine for continued benefit.
Conclusion
Exfoliating procedures can make up a large part of a skin care professional's appointments. Recognition that the pre- and post-procedure steps are as important as the exfoliating procedure itself is critical for a client to obtain the best long-term benefits.
 Dr. Carl R. Thornfeldt is President, CEO, and Chief Scientific Officer of Episciences, Inc. He is a practicing dermatologist with 24 years of skin research experience, 21 U.S. patents granted, and over 19 scientific publications in the area of treatment of skin diseases and conditions, including chapters in five dermatological textbooks. Along with these accomplishments, he has also spent nearly two decades focusing on researching the skin barrier and cutaneous inflammatory conditions. Dr. Thornfeldt received his M.D. from the Oregon Health Sciences University, and completed his dermatology residency at University Hospital, San Diego, Cali
Dr. Carl R. Thornfeldt is President, CEO, and Chief Scientific Officer of Episciences, Inc. He is a practicing dermatologist with 24 years of skin research experience, 21 U.S. patents granted, and over 19 scientific publications in the area of treatment of skin diseases and conditions, including chapters in five dermatological textbooks. Along with these accomplishments, he has also spent nearly two decades focusing on researching the skin barrier and cutaneous inflammatory conditions. Dr. Thornfeldt received his M.D. from the Oregon Health Sciences University, and completed his dermatology residency at University Hospital, San Diego, Cali
Want to read more?
Subscribe to one of our monthly plans to continue reading this article.