The field of 3D bioprinting has witnessed remarkable advancements in recent years, particularly in the development of skin models for grafting and testing. Bioprinting is the process of creating 3D living tissues using bioinks made of cells, biomaterials,and growth factors to create a microenvironment that mimics human tissue.2 It offers a groundbreaking approach to solving some of the most challenging problems in medicine, cosmetic science, and dermatology. Skin grafting is a dynamic technique of dermal reconstruction that is a crucial medical procedure for burn victims, trauma patients, and those with skin disorders.2 Additionally, 3D bioprinting plays a pivotal role in accelerating drug testing, cosmetic product development, and personalized medicine.
THE SCIENCE OF 3D BIOPRINTING
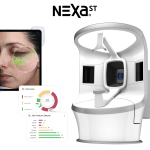
At its core, 3D bioprinting combines traditional 3D printing techniques with biological elements to create tissue-like structures. It can be done via a few fabrication techniques, like laser-based, extrusion-based, and inkjet-based bioprinting.3 Nozzle-based techniques, like inkjet and extrusion printing, and laser-based techniques, like stereolithography and laser-assisted bioprinting, are all capable of producing successful bioprinted scaffolds.3
The process begins with designing a digital model of skin, which serves as a blueprint for the printer. The bioprinter then deposits layers of bioink typically a combination of living cells and biocompatible material like hydrogels, to create skin layers.3 Each layer is carefully placed in a specific pattern to mimic the structure of natural skin, including the epidermis, dermis, and sometimes even the hypodermis, which houses the adipose cells.
Thermal inkjet uses heat-induced bubble nucleation that propels the bioink through the micro-nozzle. Piezoelectric actuator produces acoustic waves that propel the bioink through the micro-nozzle.3
The bioinks used for skin bioprinting are typically composed of human skin cells, such as keratinocytes and fibroblasts, as well as extracellular matrix materials that provide structural support. This ensures that the printed skin closely resembles human skin not only in appearance, but also in function. The result is a tissue that can perform biological functions, such as providing a protective barrier against pathogens, regulating temperature, and enabling sensory perception.
APPLICATIONS OF 3D BIOPRINTED SKIN
For Burn Victims & Trauma Patients
One of the most promising applications of 3D bioprinted skin is in the field of skin grafting. Burn victims, individuals with extensive trauma injuries, and patients with chronic conditions like ulcers often require skin grafts to repair damaged tissue. Traditional grafting techniques such as harvesting skin from a patient’s own body, called autografts, or using skin from a donor, or allografts, have limitations. Autografts are limited by the availability of healthy skin and allografts risk immune rejection,especially if the donor skin is not an exact match.
3D bioprinting overcomes these issues by creating personalized skin grafts tailored to each patient’s specific needs. For instance, researchers in Australia in the 1980s found a way to maximize skin utilization for grafting burns. This methodology evolved to a product which was approved for the market by the FDA in September 2018.1 It is approved for direct application to acute, partial-thickness thermal burn wounds in patients 18 years of age or older and application in combination with meshed autografting for acute, full- thickness thermal burn wounds in pediatric and adult patients.1
TESTING COSMETICS & PHARMACEUTICALS
Another exciting application of 3D bioprinted skin is in the testing of cosmetics and pharmaceutical products. Traditionally, testing new skin care products or drugs on human skin involved animal testing or the use of human skin samples obtained from cadavers. However, these methods raise ethical concerns and do not always accurately replicate the complexity of living, human skin.
3D bioprinted skin provides a more ethical and reliable alternative. By creating skin models that mimic the properties of real human skin, bioprinted tissue models may prove useful for screening novel compounds or predicting toxicity as the spatial and chemical complexity inherent to native tissue can be recreated.4 This is an application useful in the prioritization of lead candidates, toxicity testing, and disease models.4
PERSONALIZED MEDICINE
Personalized medicine is being developed and complemented largely by the application of bioprinting.5 3D bioprinted skin holds great promise in this area. By printing skin from a patient’s own cells, doctors can create a model that behaves just like the patient’s actual skin. This model can be applied to drug testing, toxicity in tumor treatment, and human anatomical models used to teach medical students during their studies.5
Moreover, personalized skin grafts offer a significant advantage in terms of healing and integration. Since the grafts are created from the patient’s own cells, the risk of rejection is minimized, and the tissue is more likely to integrate seamlessly with the surrounding skin. This approach also opens the door to creating personalized treatments for skin conditions such as chronic wounds, eczema, and even skin cancer, as 3D bioprinting presents itself as a promising technology to produce rapidly and reliably biomimetic cellular skin substitutes, satisfying both clinical and industrial needs.5
CHALLENGES & FUTURE DIRECTIONS
While 3D bioprinting of skin holds immense promise, several challenges must be addressed before it becomes a mainstream solution. One of the primary obstacles is the complexity of replicating the full functionality of human skin. Natural skin is a highly sophisticated organ with multiple layers and a complex vascular system that supplies nutrients and oxygen to its cells. Thus, reproducing the structural integrity and functionality of native skin to allow for wound repair, temperature control, and sensation has yet to be achieved.7 There is also a need for standardization and integration of an entire biofabrication platform, beginning with software design for building models to postprocessing of the printed tissues.6
Another challenge is scalability. While small skin samples can be printed relatively easily, creating large full-thickness skin grafts suitable for human transplantation requires advanced printing technologies and the ability to produce tissue at a scale and speed that matches clinical needs.
Despite these challenges, researchers are making significant progress. Innovation in bioinks, printing techniques, and tissue engineering are improving the quality of bioprinted skin. For example, scientists are developing methods to integrate vascular networks into printed skin which could allow for longer-term survival of grafts once implanted.
THE FUTURE IS NOW
3D bioprinting of skin is at the forefront of a revolution in medicine, offering new solutions for skin grafting, personalized treatments, and ethical testing of cosmetics and pharmaceuticals. While challenges remain, the potential benefits of bioprinted skin are immense, from speeding up recovery times for burn victims to providing personalized therapies for chronic skin conditions. As technology continues to evolve, 3D bioprinting will likely become an integral part of modern medicine, paving the way for more effective and accessible treatments for a wide range of skin-related issues.
References
- Holmes IV, J. H. (2023). A brief history of RECELL® and its current indications. Journal of Burn Care & Research, 44(Supplement_1), S48-S49.
- Ishack, S., & Lipner, S. R. (2020). A review of 3-dimensional skin bioprinting techniques: applications, approaches, and trends. Dermatologic Surgery, 46(12), 1500-1505.
- Kačarević, Ž. P., Rider, P. M., Alkildani, S., Retnasingh, S., Smeets, R., Jung, O., … & Barbeck, M. (2018). An introduction to 3D bioprinting: possibilities, challenges and future aspects. Materials, 11(11), 2199.
- Pati, F., Gantelius, J., & Svahn, H. A. (2016). 3D bioprinting of tissue/organ models. Angewandte Chemie International Edition, 55(15), 4650-4665.
- Shopova, D., Yaneva, A., Bakova, D., Mihaylova, A., Kasnakova, P., Hristozova, M., … & Semerdzhieva, M. (2023). (Bio) printing in personalized medicine—opportunities and potential benefits. Bioengineering, 10(3), 287.
- Varkey, M., Atala, A., Khademhosseini, A., & Camci-Unal, G. (2018). Current challenges and future perspectives of bioprinting. 3D bioprinting in regenerative engineering: principles and applications: Taylor & Francis.
- Weng, T., Zhang, W., Xia, Y., Wu, P., Yang, M., Jin, R., … & Wang, X. (2021). 3D bioprinting for skin tissue engineering: Current status and perspectives. Journal of tissue engineering, 12, 20417314211028574.
Dr. Zakiya M. Cush, MSTOM MPH is board-certified by the NCCAOM and specializes in cosmetic acupuncture & holistic dermatology. Dr. Cush implements Traditional Chinese Medicine and Chinese herbalism therapies to help refine the way the skin ages, thereby creating a healthy and radiant glow from the inside out. Dr. Cush is committed to educating healthcare providers and the public on dermatologic health issues related to skin of color. Sheis a certified integrative microneedling practitioner, certified aesthetic laser technician, and she successfully completed the first nationally recognized 100-hour Advanced Cosmetic Facial Acupuncture program, taught by the esteemed Dr. Shellie Goldstein, L.Ac.






























0 Comments