Equally as important is that the skin and body adapt to whatever infection or traumatic event they encounter, thereby always acting in the best interest of the body, regardless of whether or not those actions are cosmetically unappealing. Every cell is a team player and as a whole, it is a beautiful process.
A HYPERPIGMENTATION THEORY AND ITS INCONSISTENCIES
What is hyperpigmentation if it is not a damaged melanocyte? The common belief is that either through the sun, acids, or lasers, melanocytes are probably wounded at the DNA level, thereby causing them to overproduce melanin in an uncontrolled manner. The body, according to this theory, allows the melanocyte to perform abnormally for the remaining decades of its life. The primary form of hyperpigmentation is an age spot that shows up in sun-exposed areas, sometimes after the age of 30. Post-inflammatory hyperpigmentation also claims to associate with damage to the melanocyte, resulting in a perpetual overproduction of melanin as a result of DNA damage from acids or lasers.
Unfortunately, there are holes in this theory that need unraveling. Corrupted DNA triggers apoptosis if it does not become a cancerous lesion. As many know personally, most age spots never go away, nor do they turn into cancer. Therefore, it is hard to imagine the plausibility of the previously-mentioned theory because a melanocyte acting abnormally would not be allowed to survive. Virtually all cells suffer DNA damage, limiting their performance. DNA damage does not result in apoptosis. The commonly-held belief system proposes that mere damage is severe enough to cause abnormal function, which should result in cell death.
The next unexplained inconsistency relates to what happens when cells are destroyed.
Through aggressive chemical or laser peels, professionals often burn and/or explode the melanocyte as part of the treatment. The majority of the time, however, spots return within a few weeks to months, often worse than before. How can this be? How can a DNA damaged melanocyte that has been removed and replaced with an undamaged one still overproduce melanin for no reason? Some believe that the melanocyte has a memory of the damage from its brethren. This theory implies that a shared consciousness amongst cells, which is not a philosophy that is often heard from dermatologists. Textbooks describe the event simply as a replacement melanocyte. However, that theory fails to explain the recurrence of melanin overproduction. Hyperpigmentation from age spots and post-inflammatory hyperpigmentation should fit with the mechanisms associated with melasma and tanning, since one would assume cells remain consistent in their actions. Wouldn’t it be nice if everything could be explained by the same theory?
A PLAUSIBLE THEORY
Imagine that every time the skin produced excess melanin, it was doing so to protect the skin from further damage. That seems pretty logical, right? After all, melanin is specifically designed to aid the skin in protecting it from ultraviolet radiation. After age 25, every cell has some level of DNA damage that can be measured; once the cell begins to act inappropriately, it is shut down. Perhaps the DNA damage being measured in melanocytes is not related to the overproduction of melanin. It is possible that even in the case of age spots, liver spots, melasma, and post-inflammatory hyperpigmentation, the sole reason the hyperpigmentation exists is to protect the damage underneath. Instead of being a mistake, the melanocyte is purposefully acting like a melanin umbrella, providing shade from the ultraviolet light that might otherwise perpetuate the unhealed skin damage. In fact, research shows that in every instance, including tanning, there is dermal and epidermal wounding that occurs. These occurrences are likely triggering the protective action. When out in the sun for an extended period of time, the body triggers increased melanin to all the exposed areas because of the damage that was generated. The end result of this process is called a tan. Even melasma has been proven to have dermal inflammation beneath hyperpigmented areas. Post-inflammatory hyperpigmentation clearly occurs as a result of a recent wound under the skin. Age spots and liver spots also have damage that often shows as perpetual redness, once a spot has been forcefully removed with a laser or peel. This theory would certainly explain why hyperpigmentation returns to these areas even after the melanocyte is destroyed. It also explains why replacement melanocytes over many decades of life never cease to overproduce. The most compelling aspect of this theory is that it fits with what is known about the skin and body; they operate with remarkable precision and intelligence and rarely make a mistake.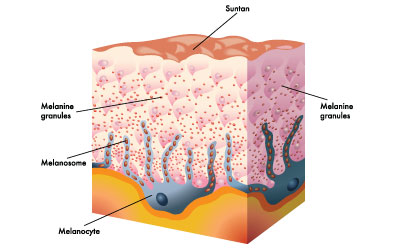
Age spots – these spots likely result from years of sun damage to the dermal-epidermal junction because it acts as the front line for ultraviolet exposure. This defense is due to the fact that the junction is the only part of the epidermis that is not replaced monthly. Wounds to the dermal-epidermal junction probably signal the closest melanocytes for support to create the umbrella of protection. An age spot is different than a freckle, which is genetically programmed, and a liver spot, which is likely dermal inflammation associated with liver damage, somewhat similar to melasma.
Tanning – this practice is another example of pigmentation and the body working perfectly. Genetically-derived skin color is based on the intensity of that person’s ancestors’ sun exposure. The creation of new melanin is triggered by exposure to ultraviolet radiation. The body hyperpigments in these areas in preparation for the next moment in the sun. This type of hyperpigmentation is more global, not unsightly, and often diminishes quickly since the damage is usually much less severe. However, severe sunburns can leave behind age spots when the dermal-epidermal junction cannot repair every aspect of that event. The key point here is that the skin intentionally increases the activity of melanocytes for protection.
Post-inflammatory hyperpigmentation – this type of hyperpigmentation is another protective response that is common after a severe wound to the skin from chemical peels or lasers. It usually occurs because the client goes outside for a prolonged period. If it persists, which may be in about half the cases, it simply means the body never completed the wound healing process in those areas. It is important to remember that wounding the skin never makes it stronger or healthier. Therefore, aggressive procedures are always at high risk of creating years of compromised skin, post-inflammatory hyperpigmentation, or worse, hypopigmentation.
MELASMA AND LIVER DAMAGE
Melasma is one of the most challenging conditions skin care professionals see today. It is commonly believed that hormone imbalances trigger certain melanocytes to overproduce. This theory presents a number of unexplainable gaps. If pregnancy-hormone levels are imbalanced as a general rule, then why are all women affected by this condition? If hormone levels are imbalanced, then every melanocyte in the body should be affected, not just small patches. After all, is not every area of skin exposed to hormones in the bloodstream? Furthermore, why does melasma occur in liver transplant and hepatitis cases? Many episodes of melasma start after a course of antibiotics or other medication for anxiety and/or depression. It is true that most cases occur in women with a history of birth control use, but what links all these different forms of hormones to creating varying patches of hyperpigmentation on the face? No one has provided any reasonable answers to these questions, yet the hormone imbalance premise persists in 99 percent of the aesthetic community.
There is a common theme that makes all this logical and allows for a more direct method of treatment: the liver. In all cases that present themselves, liver damage is a realistic source for the melasma. Obviously, transplants and hepatitis explain it. Certain antibiotics, anxiety, and depression medications are known to damage the liver. Birth control pills and any supplemental hormones can also damage the liver. How can the body, in all of its perfection, generate hormone levels in pregnancy that damage the liver? The answer comes over case analysis; most melasma cases persist in women over the age of 30. This indicates that the liver, after years of cleansing the blood of alcohol, medication, and/or general toxin exposure, is less equipped for the surge of hormones related to pregnancy. The older the pregnant client, the more likely they are to experience melasma. This theory also makes more sense with another unique aspect of melasma, because it is often temporary. Approximately two-thirds of melasma cases resolve on their own within months of delivery. This is best explained by the fact that these hormones challenging the liver are self-derived, therefore, do not cause major damage. After childbirth, the body can initiate repair of that kind of liver damage more easily than damage from harsh medication.
Liver Damage and the Face
Why does liver damage show up on the face? As Chinese medicine has shown, the face reflects all of the organ systems. Acne, rosacea, puffy eyes, and many other skin conditions can be tied to organs or different regions of the digestive tract. Liver damage tends to show up as dermal inflammation in patterns based on where damage occurs on the liver. Most of this type of damage is not picked up by typical liver function studies, so proving this theory has been based on numerous case studies and, more importantly, remarkable outcomes.
TREATMENT OPTIONS FOR HYPERPIGMENTATION
Understanding that hyperpigmentation is good for the skin until the wound is healed means that more focus should be placed on healing the wound. Instead, most skin care professionals use lightening agents and devices to expose the wound to more damage. Both daily exfoliation and peels have been shown to increase the number and severity of age spots, so this approach is not an ideal solution to the problem. Professionals have been taught that burning melanocytes destroy dysfunctional ones, which is true to some degree, depending on the severity of the peel or laser. However, professionals are also damaging the normal ones in the process, which is scientifically proven to increase the likelihood of more age spots. To be clear, the problem is not so much damaging the melanocyte as it is damaging the dermal-epidermal junction. Even under the old theory, chemical peeling and lasers are still not logical. Even daily alpha hydroxy acids, which do lighten the skin by forcing exfoliation, wound the skin and melanocyte with each application. At some point, professionals have to realize that hurting the skin in no way encourages healthy, new skin. Instead, it encourages compromised, new skin. The skin’s rate of turnover is based on its innate capacity to keep up; forcing exfoliation through increasing free radicals only serves to create an imperfect barrier and more cell damage to clean up.
Studies show that hydroquinone and retinoic acid reduce melanin production. This occurs because these ingredients poison the skin and the melanocyte. They alter its normal physiology. In no way are they treating the problem. Retinoic acid and hydroquinone are research proven to cause DNA damage, not repair it. Every ingredient that works by changing physiology or increasing free radicals will slow wound healing at every level of the skin. Even exfoliation forces the skin to go into emergency mode to repair the barrier (which is the only reason the turnover rate increases). Every year of adult life sees the skin’s nutrients decline by one percent. Therefore, forced exfoliation steals the skin’s nutrition from the dermis, which accelerates aging, and is not an ideal approach to lightening pigment. Anything that prematurely lightens a ‘melanin umbrella’ will allow for more ultraviolet damage to that area and perpetuate the problem.
Trioxolane is remarkable at repairing oxidative damage and has been shown to permanently heal age spots. While human growth factors can also help by increasing the capacity of wound repair in the skin, it is a broader solution. Vitamin C plays a role as well. The skin and body are simply trying to do what is best for the long-term health of every cell. They fix things as quickly as they can, based on the presence of the tools required. It is time to take a partnership role with the skin as skin care professionals. It is time to trust that the skin knows best. There is never a good reason to wound it.
 Ben Johnson, M.D. is the current founder and formulator of Osmosis Skincare. Dr. Johnson began his career starting one of the first medical spa chains in the country, along with founding/formulating Cosmedix. He is an established speaker, educator, and formulator who is well known for his unique approach to skin conditions by thinking outside of the box. Dr. Johnson's passion is creating tremendous change in the skin without constantly exfoliating away the protective benefits of the epidermis.
Ben Johnson, M.D. is the current founder and formulator of Osmosis Skincare. Dr. Johnson began his career starting one of the first medical spa chains in the country, along with founding/formulating Cosmedix. He is an established speaker, educator, and formulator who is well known for his unique approach to skin conditions by thinking outside of the box. Dr. Johnson's passion is creating tremendous change in the skin without constantly exfoliating away the protective benefits of the epidermis.
