Hyperpigmentation is localized excess pigmentation of the skin and can be induced by numerous intrinsic factors, including inflammatory diseases, medications, hormonal fluctuations, and the aging process. It can also be spurred on by extrinsic factors, including, most notably, ultraviolet exposure and physical or chemical wounding, which can either be accidental or brought on by therapeutic treatments, such as microdermabrasion, laser, or chemical exfoliation.
 ULTRAVIOLET RADIATION
ULTRAVIOLET RADIATION
Humans are one of a very small fraction of biological beings on Earth that are susceptible to the damaging effects of ultraviolet radiation. Skin is a natural shield that protects the entire body from damaging sun rays. Tasked with protecting the body from microbial, chemical, and physical intrusions, the skin takes the brunt of the punishment from this form of radiation, which easily penetrates the upper layers of skin.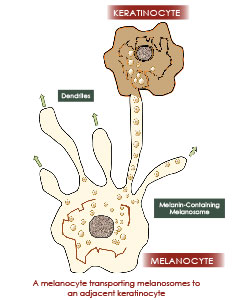
Fortunately, the skin has a natural defense system known as endogenous mechanisms that protects the skin from ultraviolet radiation and reduces or repairs any damage. Aside from the filtering effect that the stacked layers of skin cells provide, the principal protectant is the natural ultraviolet-absorbent melanin produced within the skin. In addition to its sunscreen role, which is estimated to have an equivalent SPF between 1.5 and four,1 it is also a natural antioxidant and the key definer of skin color. When uniformly distributed within the skin, it creates a youthful appearance and provides the maximum protection from ultraviolet radiation. The uniform distribution and concentration of melanin in the skin can be affected by ultraviolet radiation and chemical and microbial attacks, as well as internal processes that include hormonal fluctuations and various skin diseases. At its extreme, localized areas of the skin can either over or under produce melanin, leading to the clinical sign of hyperpigmentation or hypopigmentation, respectively.
SKIN STRUCTURE AND PIGMENTATION
To understand the production and distribution of melanin, a basic understanding of skin physiology is required. The skin is comprised of two distinctive, but interdependent, tissues: the epidermis and the deeper, highly vascularized dermis. The epidermis serves as the primary protective layer for the dermis and soft tissues beneath it and, as a result, receives the full impact of the sun's radiation. The epidermis consists principally of keratinocytes, which replicate at the basal layer, and push up to the outer surface as they mature, eventually dying and leaving a stacked layer of keratin-filled cellular envelopes that is referred to as the stratum corneum. Melanocytes sit among the young keratinocyte cells in the basal layer at an approximate ratio of one melanocyte for every 10 keratinocytes.
Melanin, which is derived from the ancient Greek word "melanos," meaning dark, are pigments biosynthesized inside the melanocyte cell from tyrosine in response to several initiating factors, including ultraviolet radiation. Tyrosine, an amino acid, is converted to L-DOPA by tyrosinase, the key enzyme that is present in the cell, and through the action of additional enzymes that produce either pheomelanin or two types of eumelanin. Pheomelanin can be characterized as a light yellow-to-red brown pigment, whereas eumelanin can be divided into black and brown pigments. Ultimately, the ratio of these pigments define skin color, with fairer skin individuals expressing higher levels of pheomelanin, red hair being one example, and darker skin and hair comprised of more eumelanin.
Once melanin is produced inside the melanocyte, it is transported out of the cell in small cellular packages called melanosomes. Melanosomes travel through branch-like appendages called dendrites, which extend from the outer surface of the melanocytes and latch on to multiple surrounding unpigmented keratinocytes and introduce pigmentation to these cells. The epidermal-melanocyte unit is typically compromised of one melanocyte attached to 30 or more keratinocytes. Studies have shown that once the pigment is inside the keratinocyte, it typically resides on the sun-facing side of the cell to protect the nucleus and its DNA from damaging ultraviolet exposure. The pigmented keratinocyte will then slowly migrate to the upper layer of skin via the natural process of desquamation and appear in the stratum corneum. This process explains why skin tanning is experienced in response to ultraviolet exposure. As one ages, the re-pigmentation of the skin in response to ultraviolet exposure slows due to a reduction in the melanocyte population. It has been estimated that 10 to 20 percent of epidermal melanocyte cells are lost by the age of 30 and drop at a rate of 10 percent per decade thereafter.2
CAUSES OF HYPERPIGMENTATION
On a biochemical level, there are two paths that can lead to hyperpigmentation. One is through an increase of melanin and melanosomes. This pathway is usually instigated by either internal stimulus, such as hormonal changes, or external irritation, such as ultraviolet or chemical exposure. The second pathway is through hyperplasia (enlargement) of the melanocyte and melanosomes, which is most often caused by sun exposure and, sometimes, idiopathically in certain disorders.
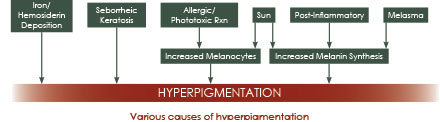
Hyperpigmentation is most commonly found to be an after-effect of inflammation in the skin. Commonly referred to as post-inflammatory hyperpigmentation, this form of hyperpigmentation can be characterized as the excess pigmentation of the skin due to a wide spectrum of inflammatory processes in response to mechanical insults such as scratches, insect bites, abrasions, cuts, acne, chemicals, or ultraviolet exposure. Inflammation can be visually detectable – such as skin erythema associated with a sunburn, healing wound, or acne – or invisible – such as low-grade ultraviolet exposure.
Inflammatory processes in the skin stimulate or introduce a wide array of biochemical signal molecules to the site of inflammation. These signals are associated with the body's complex immune response, blood clotting, and damage repair mechanisms, including cytokines, prostaglandins, and stem cell growth factors. Inflammation resulting from skin damage can provoke the release of reactive oxygen species, including superoxide and nitric oxide, and melanocyte-stimulating hormones.3,4 All of these molecular species can trigger the production of melanin and melanin transfer to keratinocytes, leading to hyperpigmentation. Considering this response, the longer an inflammatory process lasts, the more melanin deposition can occur; this reaction is often observed in chronic acne. Mitigating inflammation is key to slowing or preventing the hyperpigmentation process and re-establishing even skin color.
While hyperpigmentation is commonly associated with excess melanin deposition and/or the gathering of melanocytes in the epidermis, melanin stimulated by an inflammatory process can also migrate into the dermis, typically by being absorbed by tissue macrophages and resulting in dermal hyperpigmentation. In many cases, the tissue the hyperpigmentation appears in determines the coloration: epidermal hyperpigmentation produces a brown discoloration, deeper-seated dermal hyperpigmentation produces a blue-gray color, and a mixture of the two types creates a brown-gray appearance. When it is difficult to distinguish between the two, a Wood's lamp can be used to facilitate detection in most skin types, with the exception of Fitzpatrick types IV and V. The life cycle of melanin-filled tissue macrophages (melanophages) embedded in the deeper dermal tissue is longer than the melanin-filled epidermal cells. As a result, dermal hyperpigmentation is much more difficult to treat.
Ultraviolet Radiation
Excess exposure to ultraviolet radiation is one of the most common causes of hyperpigmentation, in addition to hormonal factors. Damage to the skin brought on by exposure to ultraviolet radiation is cumulative, although less visible in the early years of life. Freckles, one of first signs of ultraviolet exposure, are typically observed in fair-skinned and red-haired individuals and are genetically determined. These freckles, which are referred to as ephelides, are small in size – about one to two millimeters – red or light brown in color, and tend to fade with age and decreased sun exposure. The melanocyte concentration is higher in the pigmented freckle, or macule. The other type of freckle, lentigines, are larger in size, typically darker in color, and become more prominent with age, particularly after 50. Principally due to chronic exposure of ultraviolet radiation, combined with natural aging processes, solar lentigines, otherwise known as age spots or liver spots, are the most distinctive form of hyperpigmentation not only because of their color, but also because of the sharp color contrast with surrounding tissue. It is most commonly observed in individuals over the age of 60 and in body regions typically exposed to sunlight.
 Physiologically, they are best described as an accumulation of highly active melanocytes and keratinocytes packed with melanin. Studies have shown there is nearly a twofold increase in melanin and melanocytes in a pigmented lentigine lesion as compared to adjacent, normal radiation-exposed skin.3 Dermal hyperpigmentation is also associated with these spots.
Physiologically, they are best described as an accumulation of highly active melanocytes and keratinocytes packed with melanin. Studies have shown there is nearly a twofold increase in melanin and melanocytes in a pigmented lentigine lesion as compared to adjacent, normal radiation-exposed skin.3 Dermal hyperpigmentation is also associated with these spots.
Wound Healing
As part of the wound-healing process, melanocytes are stimulated to repigment the new skin cells entering the wound area. Wounding of the skin can include a thermal or chemical burn, abrasion, laceration, or even a skin-resurfacing treatment, such as chemical exfoliation. In the case of full-thickness wounds, the repigmentation process can be extremely slow as new melanocytes must slowly migrate into the healed tissue from the wound periphery, often resulting in hypopigmented scar tissue in the first weeks and months. Where hair is present, melanocytes can migrate from inside the hair follicle to repopulate the adjacent new tissue. In healthy individuals, moderate skin wounds that have disrupted the epidermis and the re-introduction of melanocytes and pigmentation occur at a faster pace.
Healing post-trauma is dependent on the critical nature of the wound, the age of the person, and the color of the person's skin. With age, the natural ability of the skin to renew itself decreases and cellular turnover slows down. Not only are less new epidermal skin cells produced, but it takes longer for them to mature. Healing time may increase from seven to 14 days in youthful skin to about 30 days in older skin. It is imperative to include cellular-renewing agents with the correct delivery systems to aid the skin's repair and regeneration mechanism.
Hormones
Hormonal changes can cause melasma, which is often associated with pregnancy or the use of medications containing artificial hormones. Melasma can be very bothersome to clients when it covers large facial areas. Common medications that can cause melasma are birth control pills and thyroid medications. In extreme cases, clients may choose to cease using these medications, causing the reversal of the pigmentation. Chloasma, or the mask of pregnancy, may manifest itself as dark patches on the face or abdomen of an expecting woman. It will typically dissipate after pregnancy, but, in some instances, it may only reduce in size. In those cases, topical treatments to lift and remove it, such as professional peels, are recommended.
Diseases and Drugs
Addison's Disease is a hormonal disease caused by insufficient adrenal sufficiency, a symptom of which may be hyperpigmentation. Diabetic clients with high insulin levels may also exhibit a specific type of hyperpigmentation. Furthermore, hemochromatosis or excess iron in the blood may also instigate skin darkening. Hyperthyroidism, another hormonal disease caused by an overproduction of thyroid hormones, may also cause hyperpigmentation. In addition to diseases, many drugs also cause hyperpigmentation. Hormonal medications and some antibiotics are some of the common drugs that can lead to irregular pigmentation.
HYPERPIGMENTATION TREATMENTS
There are a wide spectrum of treatments for hyperpigmentation. From topical treatments to energy and light treatments performed by physicians, one or a combination of treatments may be used to treat hyperpigmentation. 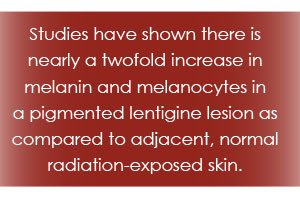
Topical treatments for hyperpigmentation can be categorized into four basic methods. They can inhibit tyrosinase, which is responsible for the synthesis of melanin; disrupt melanosomal transfers of melanin from melanocytes to keratinocytes; act as antioxidants to prevent photoaging due to oxidative damage; or accelerate epidermal turnover to lift and remove pigmentation.
Hydroquinone
The topical application of hydroquinone has represented the most common hyperpigmentation treatment for decades. Hydroquinone (1,4-dihydroxybenzene) is a phenolic compound that mainly exerts its effect on melanocytes by inhibiting tyrosinase. As such, it retards the production of new melanin, but has no effect on the existing pigment in the epidermis and dermis. Hydroquinone has also proven to have toxic effects including the generation of reactive oxygen species that can damage cellular membrane lipids and proteins. As a result of its potential side effects, which have included permanent depigmentation and the connective tissue disease, exogenous ochronosis, certain governmental agencies have removed it from cosmetic formularies and made it available only by prescription. In turn, topical treatments have moved towards utilizing natural ingredients that target the production of melanin and reduce the associated irritation and potential toxicity.
Arbutin
A gentler and natural pigment suppressant is arbutin. This ingredient is a glycosylated hydroquinone and can be found in many plants. It is abundant in cranberries, blueberries, bearberries, and pears. Its mechanism of action is exactly the same as described above for hydroquinone. However, due to its slow and controlled release of natural hydroquinone, it does not have the same toxic effect as hydroquinone.
Kojic Acid
A very versatile ingredient, kojic acid reduces hyperpigmentation via three of the four mechanisms. It acts as a tyrosinase inhibitor and makes the melasonomal transfer less effective. It also behaves as an antioxidant and neutralizes free radicals formed by ultraviolet radiation.
Azelaic Acid
A natural dicarboxylic acid, which selectively influences hyperactive and abnormal melanocytes, azelaic acid has been used to treat hyperpigmentation caused by hormones, sun damage, and inflammation. It appears to interfere with tyrosine in the active site of tyrosinase, thus working as a competitive tyrosinase inhibitor. It seems to be highly effective for melasma.
Polyphenols
A group of plant chemicals, polyphenols exhibit a plethora of health benefits. In fact, they are the largest group of tyrosinase inhibitors. They are classified into six major groups: flavones, flavonols, flavanones, isoflavonoids, flavanols, and anthocyanins. These various polyphenol groups have varying degrees of melanin inhibition. Some promising chemicals within each category include quercetin, pycnogenol, mulberry fruit, and resveratrol.
 Antioxidants
Antioxidants
Vitamins A, B, C, and E are powerful antioxidants that protect the skin against oxidative free radicals and control irregular pigmentation. Vitamin A retinoids will accelerate epidermal turnover to reduce existing hyperpigmentation. Vitamin B niacinamides inhibit melanosomal transfer to reduce pigment from spreading into neighboring keratinocytes. Vitamin C ascorbates interfere with melanin synthesis at various oxidative steps during the pigment production process. Vitamin E tocopherols inhibit tyrosinase to reduce melanin formation.
Resurfacing Peels
In order to speed up the desquamation process, several resurfacing agents can be used. These agents range from carboxylic acids – including the alpha hydroxy, glycolic, and lactic acids – to beta hydroxy acids – including salicylic acid. In addition to acid peels, retinoids are also very effective in speeding up the epidermal turnover process and, as a result, accelerate the lift off of the hyperpigmented epidermal cells. Resurfacing agents are the most effective for epidermal hyperpigmentation, especially when used in combination with a good
pigment-suppressing and sun protection regimen. Dermal hyperpigmentation, on the other hand, calls for more aggressive modalities.
Laser and Light
Both pigment-erasing laser and IPL emit specific wavelengths that can treat deeper hyperpigmentation. Medical practitioners often combine chemical resurfacing with the following two modalities to augment results:
IPL – Pulses of intense light in wavelengths between 515 and 1,200 nanometers are transmitted into the tissue. Each specific wavelength targets various chromophores in the skin, including vascular, hair, and pigment. The strong light beams help to break down the melanin.
Pigment Erasing Laser – Laser, or energy with specific wavelengths to break down melanin, are applied to the skin. It is recommended for melasma, sun damage, and post-inflammatory hyperpigmentation. For most skin types, pigmented areas darken at first, but then begin to peel within seven days.
Hyperpigmentation is a very complex skin care issue and, therefore, requires more than one simple solution. Instead of using one repetitive treatment, it is often best to combine a series of different peels along with physical modalities to treat hyperpigmentation. The less the downtime and inflammation, the better the results. Most importantly, it is imperative that any skin care professional that attempts to correct hyperpigmentation, make an even greater effort in preventing future hyperpigmentation via a daily pigment-
control regimen.
References
1 Brenner, M. & Hearing, V.J. (2007). The Protective Role of Melanin Against UV Damage in Human Skin. Photochemistry and Photobiology, 84(3), 539-549.
2 Whiteman, D.C., Parsons, P.G., Green, A.C. (1999). Determinants of Melanocyte Density in Adult Human Skin. Archives of Dermatological Research, 291(9), 511-16.
3 Ortonne, J.P. & Bissett, D.L. (2008). Latest Insights into Skin Hyperpigmentation. Journal of Investigative Dermatology. 13(1), 10-14.
4 Praetorius, C., Sturm, R.A., & Steingrimsson, E. (2014). Sun-Induced Freckling: Ephelides and Solar Lentigines. Pigment Cell & Melanoma Research, 27(3) 339-350.
 As CEO and founder of Ecozone, Inc. and Dermaware® Bio-Targeted Skin Care, Gül Zone has combined her biomedical-formulary background and cosmetic-marketing expertise to develop a line of skin and body products for aesthetic and medical practitioners. As a biochemist who has contributed to the development of several international skin care lines, Zone brings both the passion for her work and the knowledge of her formal education to her classes. Her expertise and her ability to present complex science in easy-to-follow terms allows seminar attendees to gain both practical and hands-on knowledge.
As CEO and founder of Ecozone, Inc. and Dermaware® Bio-Targeted Skin Care, Gül Zone has combined her biomedical-formulary background and cosmetic-marketing expertise to develop a line of skin and body products for aesthetic and medical practitioners. As a biochemist who has contributed to the development of several international skin care lines, Zone brings both the passion for her work and the knowledge of her formal education to her classes. Her expertise and her ability to present complex science in easy-to-follow terms allows seminar attendees to gain both practical and hands-on knowledge.
