What is less discussed are the changes that happen to the skin during the nine months of pregnancy, as well as the following months. While many clients may experience a “pregnancy glow” as hormones surge, others may notice a resurgence of acne or darkened skin on the forehead, cheeks, and chin, lengthening stretch marks on the stomach, and other skin-related conditions. A big challenge for a pregnant woman is the restriction on certain ingredients that are in place for the safety of the unborn child. Learning about the common pregnancy-related skin concerns, as well as the ingredients and products to use and avoid, will help the skin care professional ease expecting and new mother concerns in this important time of her life.
Conditions that arise during pregnancy, with which a mother-to-be may not have previously dealt, include acne breakouts and hyperpigmentation. Setting realistic expectations for the pregnant client so that they can anticipate these challenges is bound to bring them solace. It is important to note that clients should consult with their obstetrician prior to beginning any skin treatments, as many physicians have radically different feelings about ingredients to avoid and those that are safe.
 Acne
Acne
Although acne is often associated with the high school years and general adolescence, it can also arise with other hormonally-related changes in the body, including the use of birth control pills and, of course, pregnancy.
Similar to hormonal fluctuations during puberty, those that occur during pregnancy can trigger a chain reaction beginning with the enzyme responsible for converting testosterone into dihydrotestosterone, 5-alpha reductase. Androgen receptors located at the base of the follicle become stimulated by dihydrotestosterone, which in turn leads to growth in the size of the sebaceous glands, followed by increased oil production. This combination can create a plug (microcomedo) in the follicle, leading to breakouts.
Hormonally-driven acne breakouts can be unpredictable and difficult to control. In order to treat this particular concern properly, consistent care is essential. The challenge for the pregnant client is that many of the commonly-used ingredients to treat acne are considered off-limits during this time. Although many physicians recommend a longer list of ingredients to avoid, it is widely accepted that retinoids, salicylic acid, and benzoyl peroxide should be avoided during both pregnancy and lactation. If treating a pregnant, acneic client, azelaic acid and alpha hydroxy acids can be recommended. A daily regimen might look like the following:
- A cleanser with gluconolactone or alpha hydroxy acid.
- An alpha hydroxy acid-based toner with antioxidants and anti-inflammatory ingredients.
- Corrective serums with azelaic, kojic, and lactic acids, and licorice extract.
- A moisturizer that is both antibacterial and anti-inflammatory.
- A lightweight, broad spectrum sunscreen formulated for acneic or breakout-prone skin.
- Weekly: a clay-based mask with micro-fine pumice to exfoliate and rid the skin of impurities.
 Melasma
Melasma
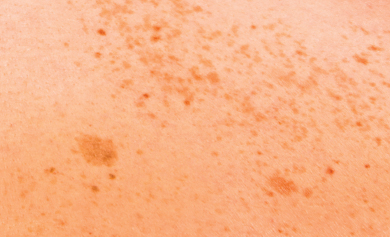
While contraception use, hormone replacement therapy, perimenopause, and thyroid disruptions can lead to melasma, this condition is colloquially known as the “pregnancy mask” due to the hormone fluctuations during pregnancy. This frustrating and difficult-to-treat condition presents with large, dense patches of pigmentation, most often on the forehead, upper lip, cheeks, and chin.
There is a general lack of knowledge about the etiology of melasma, although several studies demonstrate that patients with the condition have melanocytes with more dendrites that produce and distribute more melanosomes to their keratinocytes. Other studies point to the following as potential causes: larger and more darkly pigmented melanocytes, an increase in the number of estrogen receptors in the melanocytes, and a possible vascular component. Patients with this condition show increased melanin present, both epidermal and dermal, and more neurotrophin activity. Not only do neurotrophins boost neuron growth, but they may also trigger the process of melanogenesis.
Melasma seems to have an internal trigger, but it is also extremely sensitive to ultraviolet exposure and thermal heat. Additionally, because hormone fluctuations increase photosensitivity in many pregnant women, the importance of broad spectrum protection from ultraviolet rays cannot be overstressed to
the client.
Some may experience ‘mixed melasma’ when the pigmentation lies not only on the epidermis, but deeper in the dermis as well. Both these factors compound the difficulties in treatment. Lifting the pigment effectively, however, is possible and largely depends on consistency, much like acne. A progressive approach, as opposed to one that is more aggressive, is a must as over-treatment can easily exacerbate the condition. One of the most common ingredients used to treat hyperpigmentation, hydroquinone, is contraindicated during pregnancy. Among the best ingredients to utilize when treating melasma during pregnancy and lactation are the following: arbutin; azelaic, kojic, and lactic acids; resveratrol; rumex, licorice, and mulberry extracts; hexylresorcinol; hydroxyphenoxy propionic acid; undecylenoyl phenylalanine; and phenylethyl resorcinol.
Due to the complexity of melasma, a blend of several of the stated ingredients is recommended in a daily regimen to address the pigment pathway at multiple points and ultimately achieve success in treatment. Consider the following:
- A cleanser or cleansing
- bar with azelaic and kojic acids to promote an even skin tone.
- An alpha hydroxy acid-based toner with antioxidants and anti-inflammatory ingredients.
- Corrective serums and creams with hexylresorcinol, hydroxyphenoxy propionic acid, undecylenoyl phenylalanine, or phenylethyl resorcinol for an even skin tone, as well as antioxidants like glutathione or silybin.
- A broad spectrum sunscreen with high percentages of zinc oxide to protect the skin from ultraviolet rays, as well as potent antioxidants like caffeine.
 Dermatitis
Dermatitis
A common condition for many pregnant women is eczema, a type of dermatitis that presents as inflamed, often itchy patches of skin on various areas of the body. Of those who experience this issue when pregnant, only 20 to 40 percent have a history of eczema pre-pregnancy, the majority develop the condition it for the first time once their hormones shift. Twenty-five percent of those who have a history of eczema may experience improvement while pregnant, while 50 percent may see a worsening in the first two trimesters.
The cause of eczema flare-ups during pregnancy are thought to be due to the Type 2 T helper cell response in pregnant women, which studies show assists in normal pregnancy; at the same time, this response is related to a predisposition to allergic diseases, including atopic dermatitis. Another type of dermatitis that typically flares during pregnancy is keratosis pilaris. The red, often itchy lesions found on the back of the arms, thighs, and buttocks are caused by dry skin that traps the hair within the follicle, causing inflammation and irritation.
Should any of these conditions present during pregnancy, there are several topicals that can be provided to ease the discomfort of symptoms, including emollients like lactic acid, shea and cocoa butters, squalene, olive fruit oil, jojoba seed oil, and mild topical steroids combined with moisturizing creams. There are also serums containing ingredients like hyaluronic acid, urea, and glycerin that can help hydrate the skin deeply and minimize discomfort.
 Stretch Marks
Stretch Marks
Nearly all pregnant women experience stretch marks somewhere on their body during this period of time as their skin stretches to accommodate their growing child; 90 percent of all women will see this occur. As a result of this stretching, not only will stretch marks appear, but the mother-to-be will often experience dryness and itchiness in the abdomen area. Relief for these common concerns comes in the form of lubricating the skin on the abdomen and the rest of the body from the beginning and throughout pregnancy with rich, moisturizing topicals. A therapeutic moisturizer containing 12 percent lactic acid is a good choice to hydrate and relieve this discomfort. Additionally, daily application of shea and cocoa butters, along with products that contain high concentrations of vitamin E, can ease the itching and could potentially reduce the severity of the residual marks.
 Red Blotches
Red Blotches
What the general public may not be aware of is that the body produces around 50 percent more blood during pregnancy than other times of a woman’s life. As a result, blood vessels tend to become more visible, causing apparent redness often seen in red blotches on various body parts. Should a client present with such reddened areas, evening primrose oil, bisabolol, and red and brown algae can be used topically to help decrease vessel dilation.
While less common, some women will also experience redness and itching on the soles of their feet or the palms of their hands as a result of increased estrogen production. The same ingredients and moisturizers used to ease these conditions on the stomach can be used on these areas as well.
It is important to note that rashes, dryness, and itchiness are sometimes signs of more serious conditions. If a client is experiencing these symptoms, they should see their physician or obstetrician, especially when accompanied by loss of appetite, nausea, vomiting, or yellowing of the skin.
Avoidances During Pregnancy
Not all topical products are recommended for use during pregnancy, because studies have yet to be conducted to prove their safety. As one can imagine, not many women volunteer to be test subjects while pregnant. As a result, the following ingredients are typically contraindicated during both pregnancy and lactation: retinoids, benzoyl peroxide, salicylic acid, hydroquinone, and high-percentage alpha hydroxy acids.
While many topical skin care products do not penetrate deep enough to get into the bloodstream, some are known to be teratogens, or ingredients that can disrupt the normal development of a fetus if taken orally. Most topically-applied products do not penetrate deep enough into the skin to reach the bloodstream. That said, most obstetricians err on the side of caution with their patients during pregnancy for obvious reasons.
 Post-Pregnancy Skin Care
Post-Pregnancy Skin Care
In some circumstances, once hormone levels return to normal, the aforementioned concerns may go away on their own without intervention; other times, without the help of certain products and treatments, they may not.
Once a mother has given birth to her child and has stopped breastfeeding, it is safe to reintroduce the aforementioned ingredients that were avoided during pregnancy, as long as she has no allergies to said ingredients. This is also the time to begin reintroducing professional treatments.
Monthly in-office chemical peels can help increase cellular turnover, which will help both acne and melasma, as well as decrease bacteria and oil production, which is essential for clearing acneic breakouts. Consider modified and enhanced Jessner’s solutions, as well as salicylic acid-based treatments.
Specifically, for melasma, adding a corrective serum with hydroquinone into their daily care regimens should be considered, as well as a nightly treatment product with 0.5 percent retinol. Hydroquinone is considered a gold standard in treating hormonally-induced hyperpigmentation, while retinoids are known to inhibit neurotrophin overproduction, a key component of melasma.
These ingredients should also be used in professional treatments every three weeks for proper cellular turnover and to lift the pigment quickly, without causing undue inflammation. Consider a peel with hydroquinone, salicylic, lactic, and trichloroacetic acids formulas that are blended with azelaic, kojic, and lactic acids. Boosters and peels containing retinoids are also a good choice. In addition to hydroquinone, a client’s post-pregnancy and lactation regimen should also include serums that contain the melanogenesis-inhibiting ingredients previously mentioned, if necessary.
Make clients aware of the difficulty in treating melasma and note that it may or may not correct itself once their hormones return to normal. If someone is prone to hyperpigmentation and melasma, it can present itself again if hormones become imbalanced with another pregnancy or as menopause begins; ultraviolet exposure is always a trigger of hyperpigmentation as well.
For those who continue to experience eczema symptoms post-partum, continuation with emollient creams is recommended, along with topical steroids if necessary. For severe cases, more aggressive steroids can be considered.
As far as the red blood vessels that may remain visible post-pregnancy, clients can be counseled on the benefits of laser treatments for this condition. There are a variety of lasers that can be or are used to either lighten or remove unwanted, visible blood vessels in the skin. By flashing a pulse of light that is absorbed by the vessels and becomes heated, the body reacts as though the vessels are injured, reabsorbing them over a period of time.
Even though a mother may no longer be pregnant or lactating, it may take time for her hormone levels to return to baseline, meaning skin dryness, rashes, acne, and melasma may linger. Assure her that this is completely normal. As always, when treating any condition, emphasize the need for consistent daily care, including broad spectrum ultraviolet protection, along with monthly treatments in order to provide the most optimal outcome.
References
Weatherhead, S., Robson, S.C., Reynolds, N.J. (2007). Eczema in pregnancy. Pregnancy Plus, 335(7611), 152-154.
Unwanted Blood Vessels. Cosmetic Dermatology & Laser Center. University of Michigan Department of Dermatology. 2011-2015.
 Jennifer Linder, M.D., serves as Chief Scientific Officer for PCA SKIN®, guiding all product development and clinical trials for the company. A board-certified dermatologist and a fellowship-trained skin cancer surgeon using the Mohs micrographic technique, Dr. Linder is one of the foremost U.S. experts in the use of the cosmetic filler, Sculptra. She holds a clinical faculty position in the Department of Dermatology at the University of California,
Jennifer Linder, M.D., serves as Chief Scientific Officer for PCA SKIN®, guiding all product development and clinical trials for the company. A board-certified dermatologist and a fellowship-trained skin cancer surgeon using the Mohs micrographic technique, Dr. Linder is one of the foremost U.S. experts in the use of the cosmetic filler, Sculptra. She holds a clinical faculty position in the Department of Dermatology at the University of California,
San Francisco.
Want to read more?
Subscribe to one of our monthly plans to continue reading this article.