Causes:
 Genetics
Genetics
Acne is caused mainly by inflammation of the pores due to a combination of factors, including the production of sebum, or oil, the attraction and accumulation of bacteria, and the trapping of dead skin cells and debris within the pore. Genetics, as with most things relating to your body and health, play the largest role in which individuals are predisposed to developing acne and which are not. Those descendants of Spanish ancestry possess a gene which makes them more likely to develop a severe, cystic form of acne than other races.3 This trait can be followed in families of patients who seek treatment for themselves, then their children, and eventually, their grandchildren (Figure 1).
Hormones
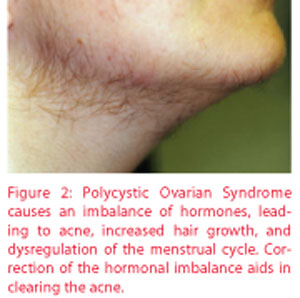
The amount of oil produced is also regulated hormonally, with higher circulating levels of testosterone generally contributing to increased amounts of oil production. However, any shift or imbalance in hormone levels can result in breakouts as well, such as commonly experienced by both sexes during puberty, and by women during their pre-menstrual cycle or during menopause. Some women suffer from polycystic ovarian syndrome (PCOS), which causes an imbalance of the sex hormones which can cause changes in the menstrual cycle, weight gain, excess hair growth, infertility, and acne, among other symptoms (Figure 2). Blood tests are necessary to diagnose this disorder, which is often treated with birth control pills to regulate the hormones.4 The acne can improve significantly upon regulation of the menstrual cycle.
 Recently, a study was done evaluating the prevalence of thyroid disorder in women with post-menopausal acne. Researchers discovered that when compared with healthy controls, women with post-menopausal acne have higher levels of antithyroglobulin antibodies.5 This might possibly indicate a link between acne and thyroid autoimmunity, and should be investigated in women displaying symptoms of hypothyroidism, which include weight gain, constipation, depression, sensitivity to cold temperatures, fatigue, heavy menstrual periods, dry brittle hair and nails, and puffy hands or feet.
Recently, a study was done evaluating the prevalence of thyroid disorder in women with post-menopausal acne. Researchers discovered that when compared with healthy controls, women with post-menopausal acne have higher levels of antithyroglobulin antibodies.5 This might possibly indicate a link between acne and thyroid autoimmunity, and should be investigated in women displaying symptoms of hypothyroidism, which include weight gain, constipation, depression, sensitivity to cold temperatures, fatigue, heavy menstrual periods, dry brittle hair and nails, and puffy hands or feet.
 Comedogenic Ingredients
Comedogenic Ingredients
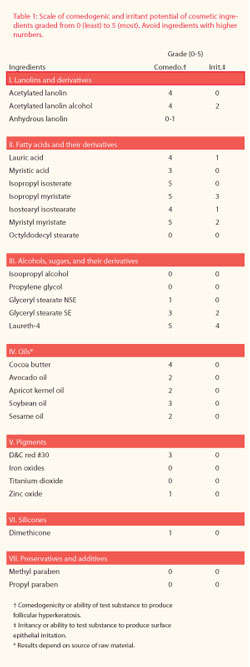
With the concern over aging, many patients are eager to rush to the cosmetics counter and purchase the thickest, richest cream they can find in the hopes that it will erase fine lines and wrinkles. Unknowingly, many of these creams contain comedogenic, pore-clogging ingredients (Table 1).6 While attempting to co-ver-up the acne, many women slather on foundations and blushes, which have dyes and other binding ingredients that make acne worse (Figure 3). Some products and chemicals cause plugging of the pilosebaceous unit or irritation reactions, which are only made worse with prolonged exposure to the skin, which is why sleeping in cosmetics is such a frowned-upon habit.
 Stress
Stress
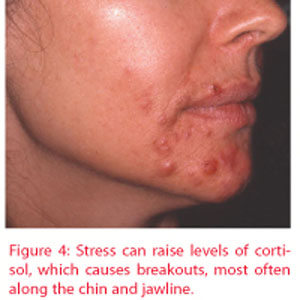
Patients suffering from severe acne report higher levels of anxiety, stress and anger than others.7,8 The reverse is also true: Stress and anxiety can cause breakouts. The mechanism lies in the hormone, cortisol, which is released by the adrenal glands in response to stressful situations. Cortisol can cause excessive sebum production and increased inflammation, both of which contribute to acne. Upon experiencing the flare-up, the patient generally reacts with even more stress, creating a vicious cycle of anxiety and acne (Figure 4). Stress also delays wound healing, necessary for the resolution of the breakout.
 Neurotic Excoriations (aka "Picking")
Neurotic Excoriations (aka "Picking")
The most difficult thing for an acne sufferer to do is to resist the urge to pick at their lesions. In some patients who have comorbidities such as obsessive compulsive disorder or high levels of anxiety, the urge is irresistible. When patients use their fingernails or other instruments to manipulate the skin, infection can be introduced, making the skin condition much worse (Figure 5). Overzealous squeezing or tugging can result in deeper impaction and even scarring. Using the nails to scratch the surface of the skin, called excoriation, is especially harmful. Discuss the implications of picking with your patients, and for those suffering also with anxiety, depression or compulsivity – psychiatric drugs can be helpful in reducing the urge to pick.
 Other Considerations
Other Considerations
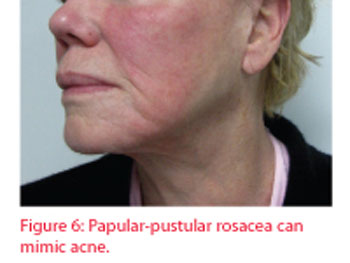
As we age, our skin barrier tends to weaken, causing a loss of moisture and an increased number of irritants to enter our skin. Many conditions can look like acne, but may not actually be. One particular condition that is frequently misdiagnosed as acne is rosacea, which in its papular-pustular form can look quite similar, although the age of onset is generally between 30 to 50 years old (Figure 6). Treatments for these two skin conditions differ; however, so it is important to see a dermatologist if you experience severe flushing or redness of the skin after consuming alcohol or spicy foods, eye irritation or if you have prominent blood vessels accompanying the papules, as these are all signs of rosacea, not acne.
An eruption of large, red-purple bumps on the face after a severely stressful life event can occur in a few genetically-predisposed individuals. This condition, called pyoderma faciale, occurs in women with an enzyme deficiency.3 It is an extreme hormone reaction to a horrific stressor, which can be detected with blood tests.
 Treatments:
Treatments:
Aesthetic Treatment
Early treatment of acne is essential, as allowing it to progress, especially cystic acne, can result in significant scarring. Patients should not attempt to express the contents of an inflamed pustule themselves; rather, an appointment should be made with a trained aesthetician or dermatologist for evaluation and proper extraction, if necessary. Attempting to extract without knowing the proper technique can cause further impaction, inflammation, dyspigmentation and scarring.
Medical Treatment
If the cause of acne is found to be hormonal, oral contraceptives or other replacements can be prescribed. As mentioned previously, if patients are suffering from co-morbid psychological conditions, anti-depressant medications can help to break the stress-acne cycle and calm patients to avoid the urge to pick at the blemishes. Topical treatment programs typically have great success in clearing the majority of patients. Oral antibiotics or isotretinoin may be indicated in some severe cases.9x
Home Care
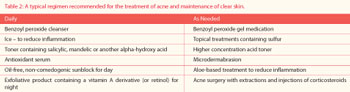
 The therapist will recommend certain products and treatments to include in the regimen which will aid in the achievement of and maintenance of a clear complexion (Table 2). There are newer cosmetics on the market today that contain skin-clearing ingredients, such as salicylic acid, to treat acne while concealing it. For many adults, acne is psychologically troublesome – participation in activities which reduce stress and boost self-esteem can be particularly helpful, such as exercising, writing, enjoying time outdoors or focusing on other enjoyable aspects which add to the quality of life.
The therapist will recommend certain products and treatments to include in the regimen which will aid in the achievement of and maintenance of a clear complexion (Table 2). There are newer cosmetics on the market today that contain skin-clearing ingredients, such as salicylic acid, to treat acne while concealing it. For many adults, acne is psychologically troublesome – participation in activities which reduce stress and boost self-esteem can be particularly helpful, such as exercising, writing, enjoying time outdoors or focusing on other enjoyable aspects which add to the quality of life.
Teenagers are not the only sufferers of acne. Well into middle age, patients can still have ranging levels of acne, from the mild comedonal acne associated with certain facial cosmetics, to the menstrual cycle papules, to the Spanish cystic acne that can plague women through menopause. By identifying the different causes of acne, we are better able to select proper treatments for patients, allowing targeted therapy for the most rapid clearing of the complexion.
Resources:
1. Knaggs HE, Wood EJ, Rizer RL, Mills OH. Post-adolescent acne.
International Journal of Cosmetic Science. 2004 Jun;26(3):129-38.
2. Addor FA, Schalka S. Acne in adult women: epidemiological,
diagnostic and therapeutic aspects. Annals Bras Dermatol.
2010 Dec;85(6):789-95.
3. Fulton JE. Acne Rx. Dutton Press, Miami, 2001.
4. Radosh L. Drug treatments for polycystic ovary syndrome.
Am Fam Physician. 2009;79:671-676.
5. Vergou T, Mantzou E, Tseke P, et al. Association of thyroid
autoimmunity with acne in adult women. J Eur Acad Dermatol
Venereol. 2011 Apr 27.
6. Fulton JE, Pay SR, Fulton JE III. Comedogenicity of current
therapeutic products, cosmetics, and ingredients in the rabbit ear.
JAAD. 1984;10:96-105.
7. Wu SF, Kinder BN, Trunnell TN, Fulton JE. Role of anxiety and
anger in acne patients: a relationship with the severity of the
disorder. JAAD. 1988 Feb;18(2 Pt 1):325-33.
8. Rapp DA, Brenes GA, Feldman SR, et al. Anger and acne:
implications for quality of life, patient satisfaction and clinical
care. Br J Dermatol. 2004 Jul;151(1):183-9.
9. Fulton JE. Acne in the adult woman. Les Nouvelles Esthetiques.
1998 Oct.
 James E. Fulton, M.D. Ph.D. is a researcher, cosmetic surgeon and dermatologist. His professional commitment to the research and treatment of skin care problems stemmed from a personal impetus, having suffered with acne through most of his childhood and early adult life. Fulton graduated from Tulane University School of Medicine in 1965. In 1972 he received a Ph.D. in Biochemistry from the University of Miami. He is currently a fellow of the American Academy of Cosmetic Surgery and American Academy of Dermatology. He is board certified. Dr. Fulton has developed skin care products for some of the leading pharmaceutical companies including Retin-A® for Ortho Pharmaceuticals along with his mentor, Dr. Albert Kligman, at the University of Pennsylvania. Fulton also developed the patented gel delivery system that stabilized benzoyl peroxide (PanOxyl®) for Stiefel Laboratories and topical erythromycin (Erygel®)for Glaxo Laboratories along with his mentor, Dr. Harvey Blank, at the University of Miami. Fulton's years of experience have culminated in the Vivant® skincare line of therapeutic products for acne, melasma and photodamaged skin. In addition to product development, he also sees patients at Flores Dermatology, Miami, Fla. and teaches Dermatology at the University of Miami.
James E. Fulton, M.D. Ph.D. is a researcher, cosmetic surgeon and dermatologist. His professional commitment to the research and treatment of skin care problems stemmed from a personal impetus, having suffered with acne through most of his childhood and early adult life. Fulton graduated from Tulane University School of Medicine in 1965. In 1972 he received a Ph.D. in Biochemistry from the University of Miami. He is currently a fellow of the American Academy of Cosmetic Surgery and American Academy of Dermatology. He is board certified. Dr. Fulton has developed skin care products for some of the leading pharmaceutical companies including Retin-A® for Ortho Pharmaceuticals along with his mentor, Dr. Albert Kligman, at the University of Pennsylvania. Fulton also developed the patented gel delivery system that stabilized benzoyl peroxide (PanOxyl®) for Stiefel Laboratories and topical erythromycin (Erygel®)for Glaxo Laboratories along with his mentor, Dr. Harvey Blank, at the University of Miami. Fulton's years of experience have culminated in the Vivant® skincare line of therapeutic products for acne, melasma and photodamaged skin. In addition to product development, he also sees patients at Flores Dermatology, Miami, Fla. and teaches Dermatology at the University of Miami.
 Caroline Caperton, M.D., M.S.P.H., holds a Master of Science degree in Public Health. She graduated with Research Distinction from the Miller School of Medicine at the University of Miami. Caperton has published extensively in the field of dermatology and is currently working as a Clinical Research Fellow in the Department of Dermatology and Cutaneous Surgery.
Caroline Caperton, M.D., M.S.P.H., holds a Master of Science degree in Public Health. She graduated with Research Distinction from the Miller School of Medicine at the University of Miami. Caperton has published extensively in the field of dermatology and is currently working as a Clinical Research Fellow in the Department of Dermatology and Cutaneous Surgery.
